[ad_1]
 BBC
BBCTechnology that identifies people at risk of a heart attack in the next 10 years has been hailed as a “game changer” by scientists.
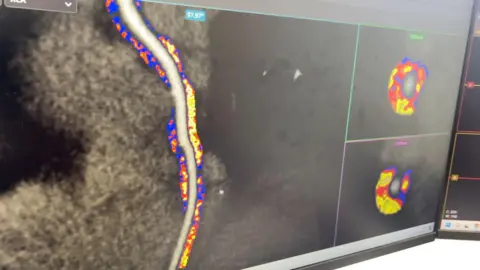
The artificial intelligence (AI) model detects inflammation in the heart that is not visible on CT scans, which involve a combination of X-rays and computer technology.
A pilot project, supported by NHS England, is running in five hospital trusts in Oxford, Milton Keynes, Leicester, Liverpool and Wolverhampton.
A decision on its use in the NHS is expected within months.
Its developer, University of Oxford spinout company Caristo Diagnostics, said it was already working to adapt the technology to prevent stroke and diabetes.
“This technology is transformative and game-changing because for the first time we can detect biological processes that are invisible to the human eye, which precede the development of narrowings and blockages (in the heart),” said Prof. Keith Channon, from the University. of Oxford.
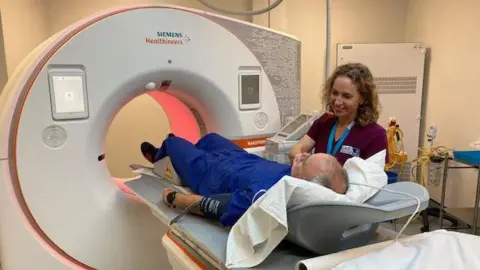
As part of the pilot, patients suffering from chest pain who are referred for a routine CT scan will have their scan analyzed by Caristo Diagnostics’ CaRi-Heart AI platform.
An algorithm, which detects coronary inflammation and plaque, is then evaluated by trained operators to verify accuracy.
Research has shown that increased inflammation is linked to a higher risk of cardiovascular disease and fatal heart attacks.
The British Heart Foundation (BHF) estimates that around 7.6 million people live with heart disease in the UK and the annual cost to the NHS in England is £7.4 billion, according to government figures .
Around 350,000 patients are referred for a cardiac CT scan each year in the UK, the BHF said.
The Orfan study (Oxford Risk Factors and Non-invasive imaging) involving 40,000 patients and published in the Lancetfound that 80% of people were referred to primary care without a defined prevention or treatment plan.
Looking at that cohort, the researchers said they found that if patients had inflammation in their coronary arteries, they had a 20 to 30 times higher risk of dying from a cardiac event in the next 10 years.
The study, funded by BHF, found that using AI technology, 45% of those patients were prescribed medication or encouraged to make lifestyle changes to prevent the risk of future heart attacks.
“wake up”

Ian Pickford, 58, from Barwell in Leicestershire, was referred for a CT scan in November 2023 after experiencing persistent chest pain.
He was enrolled in the Orphan study at the University Hospitals of Leicester NHS Trust.
The double-glazed salesman has now been prescribed statins, told to quit smoking and increase his exercise after tests using AI analysis suggested he was at risk of having a heart attack.
“It’s a big wake-up call,” Pickford said.
“And when you see it on paper, you realize how serious it is. It’s something you can look at every day and think, ‘I’ve got to do something about this.’
Professor Charalambos Antoniades, the leader of the Orfan study, said that the tools available until now were primitive because the risk calculators could only assess general risk factors, such as whether a patient is diabetic, smokes or is obese
He said: “Now, with this type of technology (AI), we know exactly which patient has disease activity in their arteries before the disease has developed.
“This means we can move earlier to end the disease process and treat this patient to prevent the disease from developing and then prevent heart attacks.”
The National Institute for Health and Care Excellence is currently evaluating the technology to determine whether it should be implemented in the NHS.
It is also under review in the United States and has been approved for use in Europe and Australia.




